Close to 4,000 Canadians will be diagnosed with oral cancer this year alone. Worldwide, more than 640,000 cases will be diagnosed. Oral cancer is a disease that primarily impacts people over 40 years of age, with men having two times greater the risk than women. It will cause approximately 800 deaths, and only approximately 57-60% of newly diagnosed cases will be alive in five years.
Oral cancer is very common in Pakistan, Taiwan, India, and in some areas of France. This is mainly attributed to tobacco and alcohol use. With increased immigration from these countries, the rate in Canada is expected to rise. In light of the growing concern about oral cancer, dentists have an important role to play in detecting this disease. It has been estimated that dentists could detect up to 85% of the cases of oral cancers each year.
The death rate associated with oral cancer is high because it is often not detected until it’s advanced stages. At this phase, the oral cancer has metastasized to another location, such as the lymph nodes of the neck, and the primary tumor has invaded deep into local structures causing severe destruction. Prognosis is very much dependent on the size of the lesion and whether there is lymph node involvement. If the lesion is less than four centimeters and has not affected the lymph nodes, then the five year survival rate is almost 90%. However, if the lesion is larger and there is lymph node involvement, then the survival rate drops dramatically to approximately 30-35%.
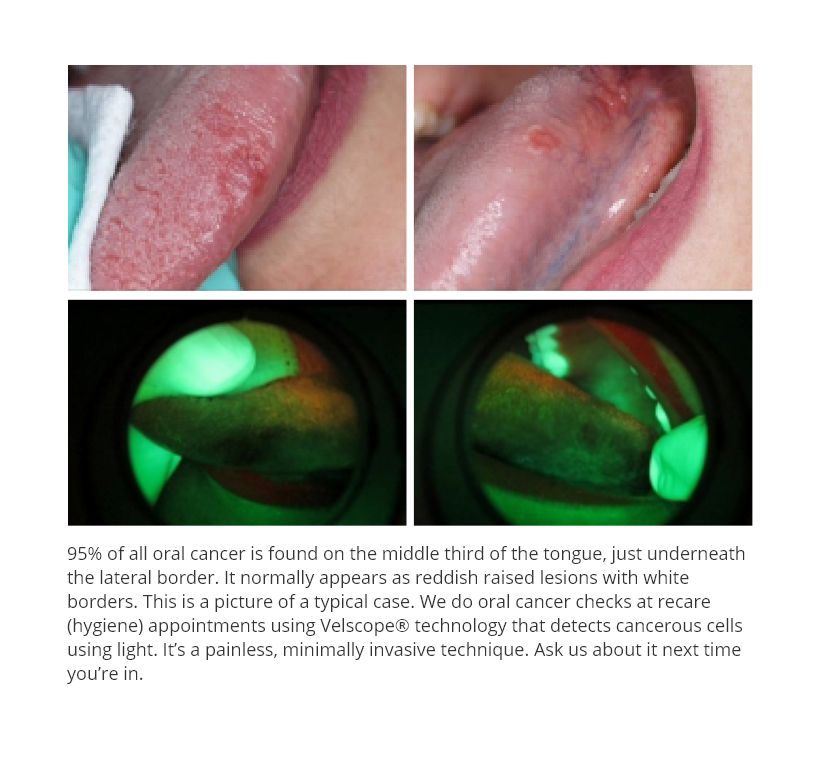
Ninety percent of all oral cancers are squamous cell carcinoma. It is mostly found on the middle third section of the tongue on the lateral border and just underneath near the floor of the mouth. It may also appear in the buccal vestibule, cheek and the palate. Another form of oral cancer is basil cell carcinoma, which is found mostly on the lower lip.
Several causes of oral cancer have been identified over the years. Tobacco is a major cause of oral cancer as both smoking and chewing tobaccos contain many known carcinogens. The risk of developing this disease is correlated with the amount of tobacco consumed and the duration of its use. Patients of South Asian background chew Betel Quid or Paan, a common habit in their culture. Betel Quid is a carcinogenic mixture, and once it is chewed, it is usually placed in the buccal vestibule for flavour.
Excessive consumption of alcohol also contributes to the risk of oral cancer. Generally, drinking 14 to 22 standard alcoholic beverages a week is considered excessive use. Tobacco and alcohol are essentially chemical factors that work synergistically, increasing the risk by more than 30 times compared to non-smokers and non-drinkers.
The Human Papilloma Virus (HPV) has been linked to an increasing incidence of oral cancer, and has played a significant role in rising incidence of oral cancer in young patients who do not use tobacco or alcohol. Of the more than 120 types of HPV, the HPV-16 and HPV-18 strains present as the primary concerns. HPV is sexually transmitted between partners and therefore impacts the younger age groups. This is the same virus that has been implicated in more than 90% of cervical cancer cases.
Individuals who have multiple sexual partners are at a much higher risk of becoming infected with HPV, which in turn increases their risk of oral cancer.
Finally, excessive exposure to the sun may cause basil cell carcinoma of the lower lip and nose primarily as a result of the UV rays, and is therefore also linked to oral cancer.
It is well known that neoplastic transformations result from mutations in genes that control cell behaviour. Mutated genes may result in a cell that divides uncontrollably, cannot repair DNA within itself, and fails to self-destruct. Several classes of genes must be mutated many times to create a neoplastic cell which then divides and grows in an uncontrolled fashion. At this stage, the cell is capable of passing the mutations to its descendants when it divides. The human body has ways to deal with or obliterate these cells, but when this process fails, cancer results.
The signs and symptoms of oral cancer vary from persistent pain, sores that do not heal (over 14 days), difficulty swallowing, slurred speech, bleeding gums, lymph adenopathy along the neck, and unilateral numbness. Detection and screening should involve a thorough review of a patient’s medical history and lifestyle habits to assess risk factors.
The two most important modifiable risk factors are the use of tobacco and alcohol. Oral cancer generally appears as a reddish raised lesion with a white border, and is sometimes ulcerated. It is usually detected visually and by touch. In the past few years, an adjunct has become available that has had very promising results. An Enhanced Oral Cancer Screening device called the Velscope Vx utilizes blue wave light spectrum which causes intra-oral tissue to fluoresce. Healthy tissue appears green in color and abnormal tissue appears dark or black. The Velscope allows dentists to diagnose dysplastic, pre-cancerous, and cancerous cells before they are visible to the naked eye. The implication of this technology is crucial: the early diagnosis of oral cancer, and much higher survival rates due to earlier treatment.
In addition to the Velscope, the Oral CDX Brush Test allows dentists to take a cell
sample much like a swab and have it analyzed. The issue with this tool is that the lesion must be visible, whereas the Velscope can detect abnormal cells before they are visible.
Oral cancer treatment usually involves a multidisciplinary approach from surgeons, chemotherapy, radiation, oncologists, dentists, nutritionists, and rehabilitation specialists.
Regular checkups that include an examination of the entire mouth can detect pre-
cancerous conditions or the early stages of oral cancer. At Bhandari Dental, screens are conducted by traditional visual and touch checks, as well as the use of Enhanced Oral Cancer Screening using the Velscope Vx.
Dr V Bhandari BSc DIH DDS
2525 Old Bronte Rd, Suite 470
Oakville, Ont L6M 4J2 www.bhandaridental.com 905-825-5110
References
1 Mayne S, Morse D, Winn D. Cancers of the oral cavity and pharynx. In:Schottenfeld D, Fraumeni J, Jr, editors. Cancer epidemiology and prevention3rd ed. New York: Oxford University Press; 2006. p.674-96
2 Canadian Cancer Society, National Cancer Institute of Canada. Canadian cancer
statistics 2007. Toronto(ON); 2007
3Piccirillo J, Costas I, Reichman M. Cancers of the head and neck. In: Ries LA, Young
JL, Keel GE, Eisner MP, Lin YD, Horner MJ editors. SEER survival monograph: cancer
survival among adults:U.S. SEER Program, 1988-2001, Patient and tumor characteristics, NIH Pub. No. 07-6215. Bethesda (MD): National Cancer Institute, SEER Program; 2007. p. 7-22
4 Lingen M, Sturgis EM, Kies MS. Squamous cell carcinoma of the head and neck in
nonsmokers: clinical and biologic characteristics and implications for management. Curr Opin Oncol 2001; 13(3):176-82
5 Hashibe M, Ford DE, Zhang ZF, Marijuana smoking and head and neck cancer. J Clin Pharmacol 2002;42(11 Supppl):1035-75
6 Bhatia S, Louie AD, Bhatia R, O”donnell MR, Fung H, Kashyap A, and others. Solid
cancers after bone marrow transplantation. J Clin Oncol 2001;19(2):464-71
7 Curtis RE, Rowlings PA, Deeg HJ, Shriner DA, Socie G, Travis LB, and others. Solid
Cancers after bone marrow transplantation. N Engl J Med 1997:336(13):897-904